Understanding Calcium: Beyond the Myths
Why Calcium Matters More Than You Think
Calcium is the most abundant mineral in your body, making up about 2 pounds of your total body weight. While 99% of it resides in your bones and teeth providing structural support, the remaining 1% plays critical roles in muscle function, nerve transmission, blood clotting, and heart rhythm regulation.
Common Calcium Misconceptions
Many people fear calcium, believing it causes arterial buildup or kidney stones. However, these problems typically occur when large amounts of calcium are taken alone or in improper ratios with other nutrients. When calcium is properly balanced with magnesium and other synergistic nutrients, it remains in solution and performs its essential functions without accumulating where it shouldn't.
The Calcium Paradox: Sometimes You Need More to Have Less
One of the most misunderstood aspects of calcium metabolism is that people with high tissue calcium levels as revealed through Hair Tissue Mineral Analysis (HTMA) often benefit from taking more calcium, not less. This seeming contradiction occurs because high tissue calcium on HTMA often indicates "biounavailable calcium" – calcium that's present but not usable by the body, accumulating in soft tissues instead of being properly utilized.
Think of it like having a clogged drain: you might have plenty of water (calcium) backing up in your sink (tissues), but what you actually need is to fix the drain mechanism (add the right cofactors) so the water can flow properly to where it's needed.
Key Signs Your Body Needs Calcium Support
This is just a short list:
Muscle cramps, especially during physical activity
Brittle nails that break easily
Dental problems
Numbness and tingling in fingers and toes
Fatigue and weakness
The Importance of Proper Ratios
Calcium doesn't work alone.
Synergistic nutrients that help calcium work better:
Magnesium (keeps calcium in solution)
Vitamin D (enhances absorption)
Vitamin K2 (directs calcium to bones)
Phosphorus (structural support)
Boron (enhances vitamin D function and reduces calcium loss)
Copper (essential for bone collagen formation)
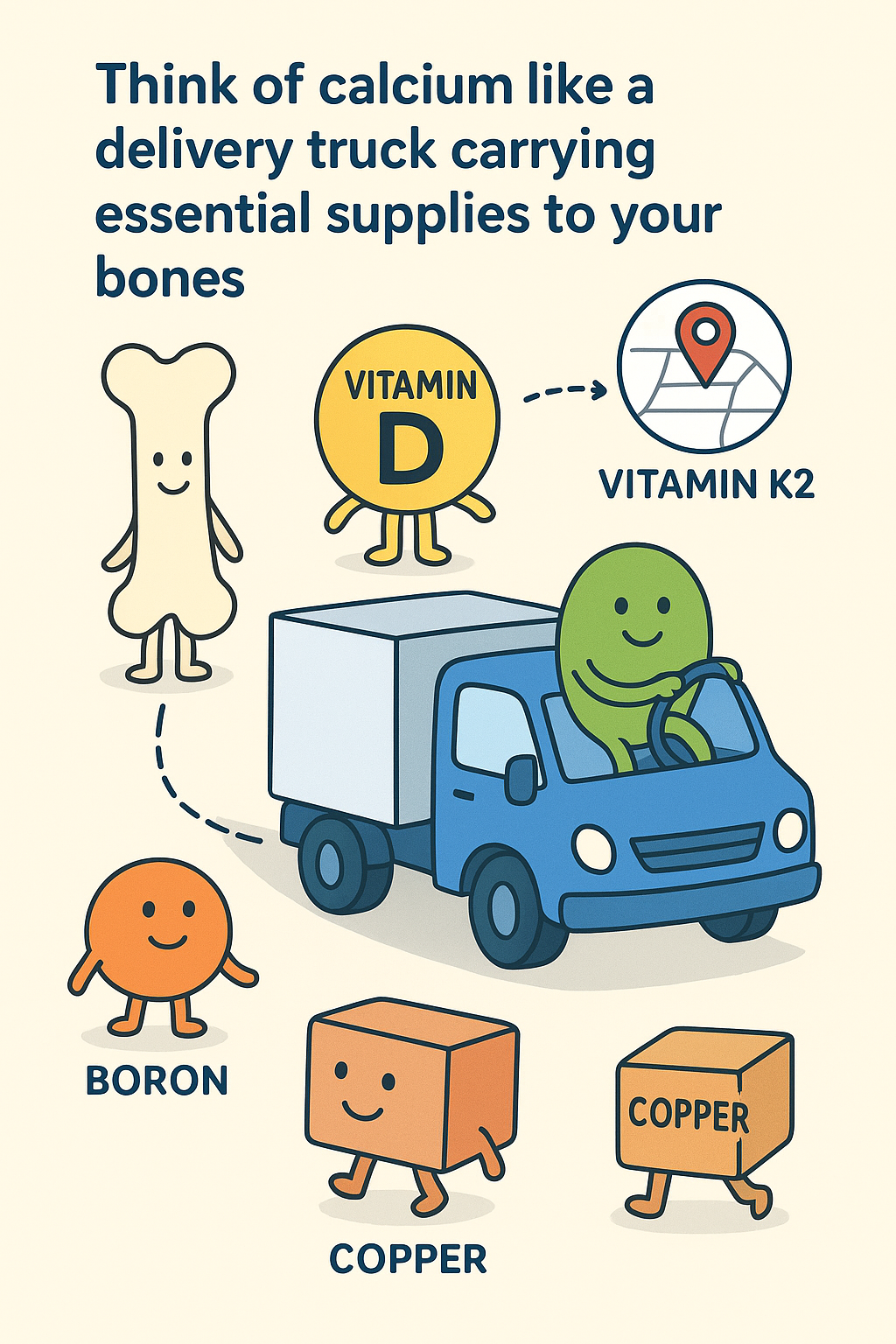
Think of calcium like a delivery truck carrying essential supplies to your bones. Vitamin D is like the loading dock that helps get the supplies on the truck, magnesium is the skilled driver who knows how to navigate properly, and Vitamin K2 is the GPS system that ensures the truck arrives at the right destination (your bones, blood, etc..) instead of getting lost and dumping its cargo in the wrong neighborhood (soft tissues). Meanwhile, boron acts like the fuel efficiency system that helps the truck run longer and waste less fuel, while copper provides the construction materials needed to build strong foundations once the delivery arrives.
Why magnesium is crucial: Magnesium keeps calcium in an ionized, useable state and prevents it from accumulating inappropriately in soft tissues. This is why we use quality calcium supplements that include magnesium in proper ratios.
Boron helps enhance bone health by increasing how long vitamin D works in your body and influences the metabolism of calcium, magnesium, and vitamin D.
Copper helps calcium and other minerals work more effectively and is an essential cofactor for enzymes involved in connective tissue formation, which is crucial for bone matrix development.
Excellent Food Sources of Calcium
Dairy sources: Milk, yogurt, cheese
Non-dairy sources:
Sardines and salmon
Leafy greens like kale
Almonds and sesame seeds
White beans and lentils
Figs
What Can Interfere with Calcium
Certain factors can reduce calcium absorption or utilization:
Inadequate stomach acid
Foods high in oxalates (spinach, rhubarb) when consumed in large amounts
Phosphoric acid in sodas
Excessive dietary fiber (such as from fiber supplements)
Chronic stress
The Role of Hair Tissue Mineral Analysis (HTMA)
Hair tissue mineral analysis can provide valuable insights into your calcium status that blood tests may miss. This testing can reveal whether calcium is being properly utilized or accumulating inappropriately in tissues, helping guide personalized supplementation strategies.
Imagine your blood test as a snapshot of what's happening on a busy highway at one moment in time, while HTMA is like reviewing the traffic patterns over several months. Blood tests show what's currently circulating, but HTMA reveals the long-term story of how minerals have been moving through and accumulating in your body's tissues.
HTMA also helps identify underlying factors that can significantly affect calcium levels:
Adrenal function: Weak adrenals can lead to calcium accumulation in tissues rather than proper utilization
Thyroid issues: Both overactive and underactive thyroid function directly impact calcium metabolism
Heavy metal toxicity: Metals like lead and cadmium can displace calcium and interfere with its absorption
Nutrient deficiencies: Deficiencies in key minerals like magnesium, copper, or zinc can dramatically alter how your body handles calcium
Key Takeaways
Calcium is essential for far more than just bone health
Quality matters – calcium with proper cofactors works differently than calcium alone
Individual needs vary – what works for one person may not work for another, hence HTMA testing
Trained Global Nutritional Healing practitioners understand exactly how much calcium to recommend, along with the specific cofactors and synergistic nutrients needed for your unique biochemistry
Work with a Trained Global Nutritional Healing Practitioner
Remember: calcium isn't the enemy – improper calcium metabolism is. With the right approach, calcium can be safely and effectively used to support optimal health.
References
Pizzorno, L. (2015). Barking up the wrong tree: The case for calcium supplementation. Integrative Medicine Research, 4(2), 73-81.
Saini, R., Badole, S., & Zanwar, A. (2017). The synergistic interplay between vitamins D and K for bone and cardiovascular health: A narrative review. International Journal of Endocrinology, 2017, 7454376.
Capozzi, A., Scambia, G., & Lello, S. (2020). Calcium, vitamin D, vitamin K2, and magnesium supplementation and skeletal health. Maturitas, 140, 55-63.
Uwitonze, A. M., & Razzaque, M. S. (2018). Role of magnesium in vitamin D activation and function. Journal of the American Osteopathic Association, 118(3), 181-189.
van Ballegooijen, A. J., Pilz, S., Tomaschitz, A., Grübler, M. R., & Verheyen, N. (2017). The synergistic interplay between vitamins D and K for bone and cardiovascular health: A narrative review. International Journal of Endocrinology, 2017, 7454376.
Watts, D. L. (2010). Trace Elements and Other Essential Nutrients. 3rd edition. Trace Elements, Inc.
Hair Tissue Mineral Analysis (HTMA) as analytical test for mineral composition assessment. Interclinical Laboratories. Retrieved from interclinical.com.au
Malter, R. A. (2003). The Strands of Health: A Guide to Understanding Hair Mineral Analysis. Endo-Met Laboratories.
Rimm, E. B., Willett, W. C., Hu, F. B., et al. (1998). Folate and vitamin B6 from diet and supplements in relation to risk of coronary heart disease among women. JAMA, 279(5), 359-364.
Akbulut, A. C., Pavlic, A., Petscher, C., et al. (2020). The importance of vitamin K and the combination of vitamins K and D for calcium metabolism and bone health: A review. Nutrients, 12(9), 2420.
This information is for educational purposes and should not replace professional medical advice.